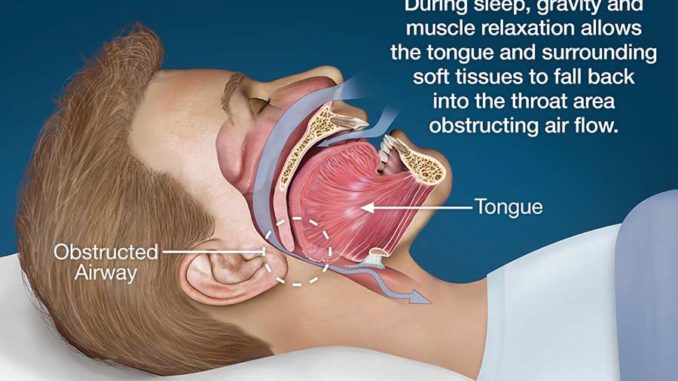
Sleep Apnea is a condition caused by a lack of air passing through to the lungs during sleep; it is an episode that lasts for more than 10 seconds. This deficiency of air leads to a decreased saturation of oxygen levels in the blood, which results in oxygen deprivation of the brain and other bodily tissues, known as Hypoxia. In order to normalize blood oxygen levels, the brain instructs a micro awakening and commands the body to reopen the airways. The person wakes up for a short time and commences breathing, often noisily at first, and then falls back to sleep. Quite often, the person has no memory of these micro-awakenings in the morning.
During sleep, the muscles of the pharynx (part of the throat that sits behind the mouth and nasal cavity) overly relax and obstruct the airway, which is what causes the Sleep Apnea episodes. Such episodes can occur several times within an hour of sleep and any more than 10-15 episodes of Sleep Apnea within an hour is Obstructive Sleep Apnea Syndrome. This syndrome divides the night’s sleep into hundreds of small fragmented mini sleeps, resulting in the person feeling exhausted as body’s systems have not had enough time to rejuvenate over night. The oxygen deficiency also affects a person’s metabolism, which is why an Obstructive Sleep Apnea sufferer wakes up tired, irritable and usually has a headache.
According to the American National Sleep Foundation, Obstructive Sleep Apnea syndrome costs the United States more than $100 billion annually. This is a very common problem, however it is not highly publicized, therefore many people are unaware of its existence.
When it comes to treatment of Obstructive Sleep Apnea, the gold standard is CPAP-therapy, which involves wearing a CPAP mask during sleep. Approximately 50% of patients do not like CPAP-therapy for a long period due to the intrusive nature of the CPAP mask. Furthermore, CPAP-therapy is not recommended for mild and moderate forms of Obstructive Sleep Apnea syndrome. So, what is the recommended treatment for this?
Sleep Apnea Dentists Can Help Treat Mild Obstructive Sleep Apnea Syndrome
Sleep Apnea Dentists can help treat mild and moderate forms of Obstructive Sleep Apnea syndrome through dental devices, which can also be used with CPAP-therapy for more effective results. The dental devices are easy to use, are compact, effective and affordable. The main function of these devices is to keep airways open to prevent the Obstructive Sleep Apnea episodes. These oral appliances have been used in medicine for nearly 30 years and have continuously improved in technology over the years. The most significant improvements have been comfort focused, namely the appearance of the device and materials used in construction.
There are three common types of dental devices worn in the mouth at night, and fitted by a dentist or orthodontist:
1) Tongue Retaining Devices (TRD)
These devices hold the tongue to ensure the airways are kept open.
2) OPA Devices (Oral Pressure Appliance)
These devices lift the soft palate (the tissue in the back roof of the mouth) and hold the tongue in a certain place to keep airways open.
3) The Mandibular Advancement Splines (MAS) or Mandibular Advancement Devices (MAD)
These are the most widely used oral devices for Obstructive Sleep Apnea syndrome. Their function is to hold the lower jaw in a forward position, thus allowing normal airflow to the lungs and preventing displacement of the lower jaw during sleep. As a result, the airflow is completely restored and the Obstructive Sleep Apnea episodes stop.
Modern Mandibular Advancement devices are individually made for the upper and lower jaws, and both are fixed to the jaws before bedtime. When attached to the jaw, this device creates an opening of the airways through the forward position of the jaw and tongue. The lower part of the device holds the lower jaw in a forward position at about 75% of the maximum forward movement. After two weeks of wearing this device, the patient undergoes a second re-examination in a sleep study. If required, the dentist can manipulate the device by moving the jaw forward several millimeters to further correct the issue.
The dental device is tailored to each person, as each mouth is unique. The methods used to ensure the correct device is made and fitted include: Cephalometry (measurement and study of the proportions of the head and face), computed tomography, magnetic resonance imaging, video endoscopy and lateral Cephalometry of the patient with and without the device in their mouth.
A dental device is usually recommended in the following situations:
1) Mild or moderate forms of Obstructive Sleep Apnea Syndrome (episodes of Apnea less than 20 within an hour);
2) A patient’s unwillingness to use a CPAP-mask or undesirable results from using it;
3) A patient’s unwillingness to do a surgical treatment or unsuccessful surgical treatment in the past;
4) Patient is in a healthy weight range (BMI- Body Mass Index is used to measure this);
5) Patient’s willingness to use the dental device every night.
What to Consider before Visiting a Sleep Apnea Dentist
Dental devices are not recommended in treating patients with Central Sleep Apnea Syndrome, as this type of sleep Apnea is not associated with the narrowing of the upper respiratory tract, rather is it closely related to heart and lung issues.
For patients with severe forms of Obstructive Sleep Apnea syndrome, the oral device is not enough, and such patients are treated with CPAP-therapy.
There are also age restrictions; the oral devices are not suited to patients less than 18 years of age.
Diseases of the temporomandibular joint (the sliding joint that connects to jawbone to the skull) are quite common among patients with Obstructive Sleep Apnea syndrome. However, today there is no reason to discourage the use of dental devices in patients with this disease. Studies show that side effects, such as pain in the temporomandibular joint and chewing muscles are rare, usually weakly expressed and often only occurs in the initial stages of using the dental devices.
Bruxism is a more common disease among patients with Obstructive Sleep Apnea syndrome. In such cases, the use of oral devices helps prevent abrasion of teeth and significantly reduces the motor activity of the chewing muscles during sleep.
According to the latest data, it was found that:
• Many patients prefer to use oral devices with and without CPAP-therapy- 56-68% of patients continue to use oral devices for more than 30 months;
• The effectiveness of the devices depends on the design and manufacturing;
• Side effects of the use of devices are common but not critical- mainly salivation, uneasy sensations in the chewing muscles and discomfort for teeth at the beginning of treatment.
Proudly WWW.PONIREVO.COM



